How To Train Your Pelvic Floor
First, what exactly is the pelvic floor and why is it important?
The pelvic floor is a group of muscles that provide support around your bladder, bottom and vagina. One of the key functions of your pelvic floor muscles is to support healthy continence, giving you control over when you go to the bathroom. They’re also important for maintaining posture and stability, and have even been linked to sexual performance and pleasure. If your pelvic floor muscles are weak, you may find you leak urine when you cough, sneeze or strain. This is quite common, and there is no reason to feel embarrassed if it does happen.
Is there anything you can do before giving birth to help strengthen it?
For pregnant women, training the pelvic floor muscles will help their body support the weight of a growing baby. It will also help muscles recover more easily once the baby is born. It’s a good idea for most pregnant women to consider pelvic floor exercises, even if they’re young and not suffering from stress incontinence just yet. Generally speaking, alongside your pelvic floor exercises, deep abdominal exercises like swimming, walking, and Pilates are all good. But it’s always worth speaking to a healthcare professional who can advise which specific exercises to do.
What about after the birth?
Do as much as you can, as often as you can. You might find fatigue and lack of sleep makes pelvic floor exercises harder, so try to fit them in around other activities, for example, when you are feeding your baby. Start as soon as you feel comfortable and as long as you don’t have any pain. If you've had a C-section, you might want to wait until your scar has healed and isn't too sore. You can also practice exercises lying down, sitting or standing.
How long should it take to feel results?
Continue doing pelvic exercises for a few months before you expect to see any noticeable results. If you find you are still leaking urine after 12-16 weeks, it would be a good idea to visit your GP or women’s health physiotherapist for further advice and treatment.
What’s your advice for women experiencing problems in later life?
There is no right or wrong time to start doing your pelvic floor exercises – it might be years after giving birth. You can start doing them whether or not you have any pelvic floor problems, like a prolapse or stress urinary incontinence. If you do have symptoms, it’s recommended you consult a women’s health physiotherapist, who can give you guidance on the specific tailor-made pelvic floor exercises to suit your needs.
How does the menopause affect your pelvic floor?
The onset of menopause can cause your pelvic floor muscles to weaken, so it is not unusual for pelvic floor symptoms to develop later on. Reduced pelvic floor muscle function around the time of menopause can also be due to weight gain, which is common during this time.
Other factors that can heighten the chances of pelvic floor dysfunction later in life are trauma resulting from childbirth, and chronic conditions such as diabetes or asthma, which can cause bladder or bowel control problems. A course of pelvic floor strengthening exercises are usually recommended before any other treatments. If there is only limited improvement after completing these exercises, then a referral to a urologist or gynaecologist can be made for alternative treatment options.
If you find the exercises aren’t working, what are the treatment options?
If pelvic floor exercises don’t work and you find you are still leaking urine, there are other treatments to try before considering surgical options. If your pelvic floor muscles are very weak or you're unable to activate their pelvic floor, electrical stimulation is an alternative. With this procedure, a small probe is inserted into the vagina, with an electrical current run through the probe to stimulate the muscles. Don't worry, t isn't painful.
Biofeedback is another option, which can be used if a person is struggling to activate their pelvic floor, as it strengthens the muscles and improves proprioceptive and sensory awareness. Like electrical stimulation, a probe is inserted into the vagina and then, once the woman activates her pelvic floor, they will get visual feedback, in relation to their contraction on the screen of the device.
Another alternative is a topical oestrogen cream, which women are often prescribed by their doctor, gynaecologist or urologist, which helps bulk up the vagina muscles post-menopause. It is recommended that this is used in conjunction with pelvic floor training. It should be said, however, that pelvic floor rehab needs to be done in conjunction with lifestyle interventions like weight management to successfully reduce stress urinary incontinence.
Do surgical procedures work?
Surgery should only be considered if all the other treatments have failed. One surgical option is a colposuspension, which is performed under general anaesthetic. Stitches are placed in the pelvis to lift the bladder neck upwards, offering a long-term treatment for stress urinary incontinence. It can take around four weeks for women to recover following this operation, with no heavy lifting or exercise for six to eight weeks.
Another option is an autologous rectus fascial sling, which involves making a cut in your abdomen and vagina to fit a sling in the neck of the bladder to support it and prevent urine leaking.
Finally, urethral bulking agents are lesser-known surgical treatments. They involve a soft, small gel injected into three or four locations in the urethral wall (the tube that urine comes out of). This procedure takes 5-10 minutes and is often carried out under local anaesthetic. It is important to discuss all these options with your consultant and find out which is best for you.

The first thing you'll need to do is find your neutral spine. To do this, sit in an upright chair with your feet flat on the floor. From there, place your knees hip distance apart and imagine your pelvis is a bucket of water.
Spill the bucket backward flattening your back, then spill the bucket forward creating an arch in your lower back. Move through this pelvic tilt until you find the middle point between these two positions. This is your ‘neutral’ spine position.
Inhale to prepare, exhale slowly imagining you are stopping wind coming out of your back passage and then lifting from your front passage (as if you were trying to stop urinating).
Finding your deep abdominals. Place your hands under your back below your lower tummy, inhale to prepare, exhale slowly and tighten your deep abdominals by drawing your lower tummy away from your hands a little (as if you were to zip up your trousers).
Hold both pelvic floor muscles and deep abdominals for as long as you can. Aim for 8-12 lifts and squeeze for a duration of 8-12 seconds or whatever you can do. Let go in between for few seconds, making sure you are fully relaxed. Gradually build up on how long and how many repetitions you can do.
Remember to keep breathing into your stomach (instead of just your chest) and try not to tighten your thighs or bottom when you do.
/https%3A%2F%2Fsw18.sheerluxe.com%2Fsites%2Fsheerluxe%2Ffiles%2Farticles%2F2020%2F06%2Ftry-one-these.jpg?itok=y9oOew0G)
Elvie Pelvic Floor Trainer, £152.10
This is the smallest kegel trainer and exercise tracker available. It also connects to an app that gives you feedback as you exercise, and guides you through easy-to-learn, five-minute workouts.
Available at johnlewis.com
Kegel8 Ultra 20 Electronic Pelvic Toner, £133.32
With up to 20 clinically proven pelvic floor exercises and relaxation programmes to choose from, this gadget is great for helping tackle incontinence, and is also suitable for those who have suffered with prolapse or are post-hysterectomy.
Available at kegel8.co.uk
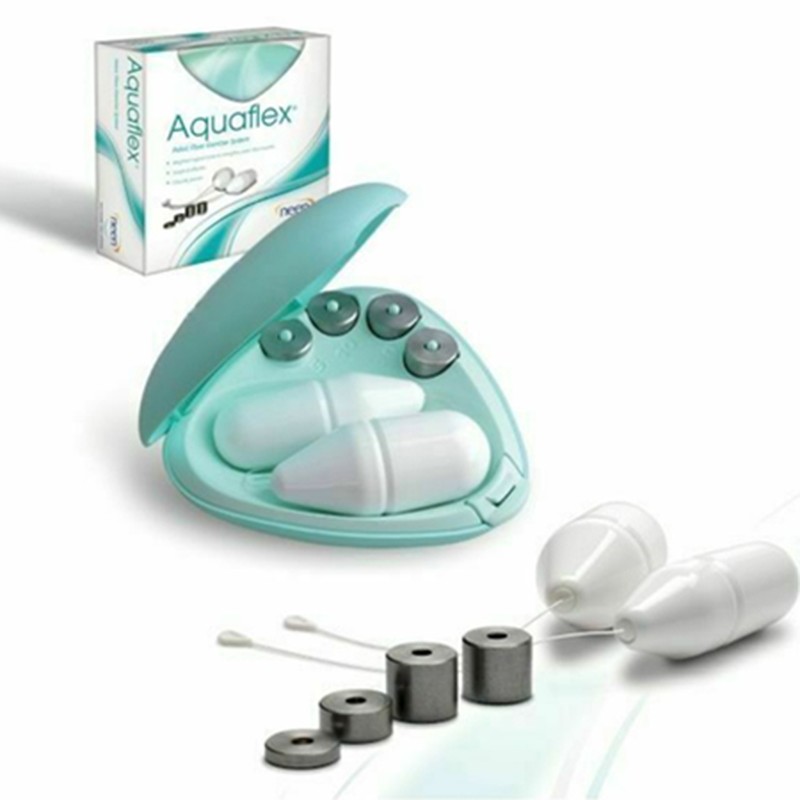
Neen Aquaflex Pelvic Floor Exercise System, £17.47
This cheap and cheerful option helps to isolate and contract the pelvic floor muscles using cones, all of which contain weights to strengthen the muscles over time.
Available at amazon.co.uk
DISCLAIMER: We endeavour to always credit the correct original source of every image we use. If you think a credit may be incorrect, please contact us at info@sheerluxe.com.



/https%3A%2F%2Fsw18.sheerluxe.com%2Fsites%2Fsheerluxe%2Ffiles%2Fwebsite-images%2F2025%2F04%2Fnew-parenting-background-image.jpg?itok=rRrLkJpg)